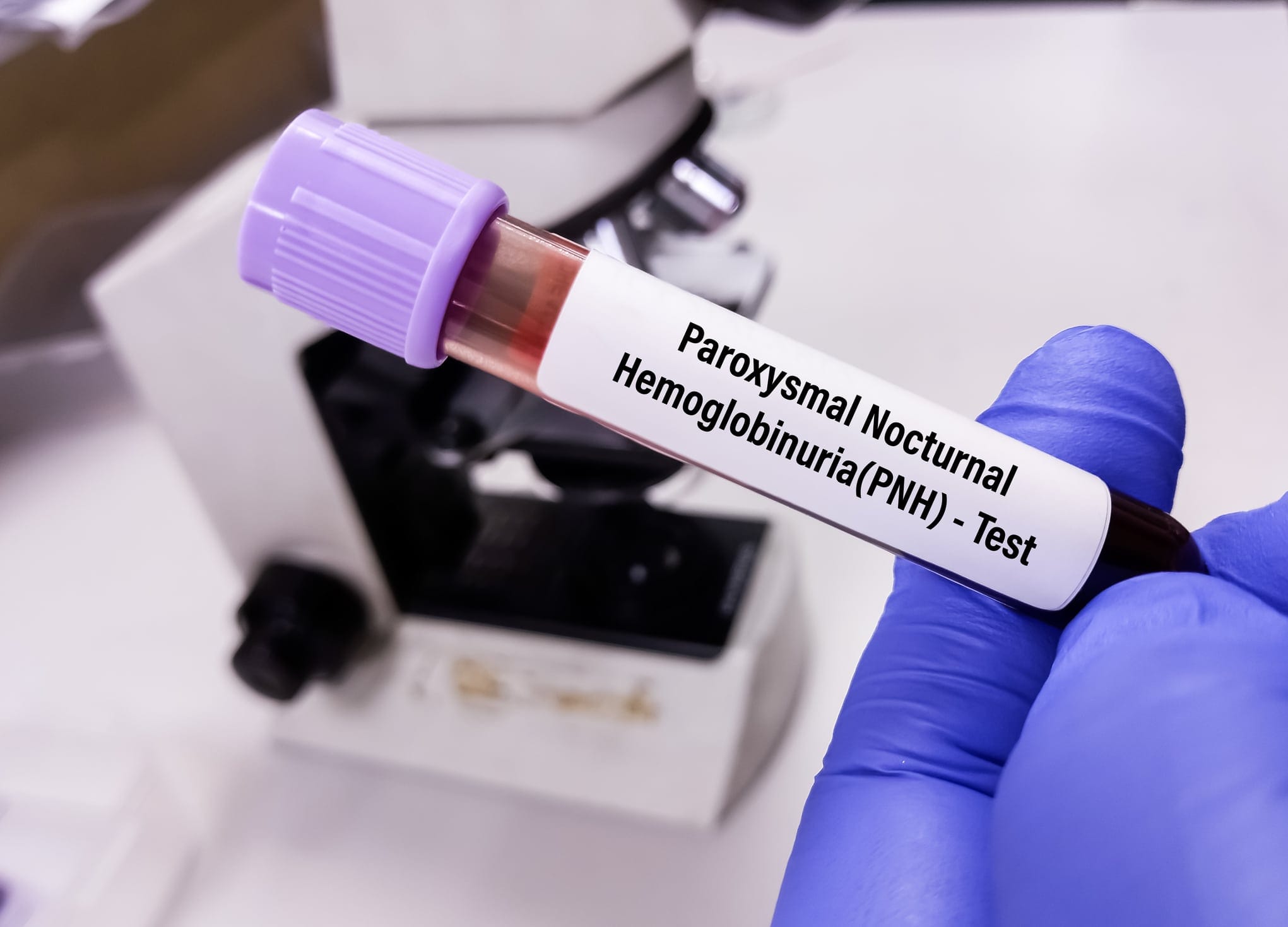
Paroxysmal nocturnal hemoglobinuria (PNH) is a rare disorder characterized by a range of unexplained symptoms. It primarily causes problems, including intravascular hemolysis, thrombosis, and bone marrow suppression. In this article, we will provide a detailed review of the evaluation and treatment of paroxysmal nocturnal hemoglobinuria.
Thank you for reading this post, don't forget to subscribe!Causes of Paroxysmal Nocturnal Hemoglobinuria (PNH)
People with this condition have blood cells that are missing a gene called PIG-A. This gene enables a substance called glycosylphosphatidylinositol (GPI) to facilitate the attachment of certain proteins to cells.
Without PIG-A, important proteins cannot connect to the cell surface and protect the cell from substances in the blood called complement.
As a result, red blood cells break down too early. The red cells leak hemoglobin into the blood, which can pass into the urine. This can happen at any time, but is more likely to occur during the night or early morning.
The disease can affect people of any age. It may be associated with aplastic anemia, myelodysplastic syndrome, or acute myelogenous leukemia.
Signs and Symptoms of Paroxysmal Nocturnal Hemoglobinuria (PNH)
-
- Intravascular hemolysis, anemia, fatigue, and dyspnea are among the symptoms.
- Inadequate bone marrow activity can cause aplastic anemia in certain conditions.
- Free hemoglobin is released during hemolysis, which overloads clearance processes and reduces nitric oxide.
- Smooth muscle dystonia, dysphagia, esophageal spasm, and abdominal pain may occur from reduced nitric oxide.
- Accumulation of iron and acute kidney disease induced by chronic hemolysis can result in hemosiderosis, which can be fatal.
- Defective fibrinolysis, nitric oxide depletion, inadequate complement activation, and GPI anchor protein deficiency all lead to approximately 40% of PNH patients experiencing thrombosis.
- In addition to symptoms including dark urine, easy bruising or bleeding, headache, shortness of breath, weakness, fatigue, pallor, and chest discomfort, some individuals might experience blood clots, back pain, and abdominal pain.
Diagnosis and Tests for Paroxysmal Nocturnal Hemoglobinuria (PNH)
Flow cytometry → It uses antibodies to glycosylphosphatidylinositol-anchored proteins (GPI-AP) is the most accurate technique for diagnosing PNH.
To rule out hereditary problems, it is suggested to first quantify at least two GPI-APs. The test identifies GPI-AP-deficient cell types, estimates the percentage of defective cells, and divides them as PNH III (full deficiency), PNH II (subtotal deficit), or PNH I (normal expression). Knowing the amount and type of deficient red cells helps to manage PNH-related anemia.
Complete Blood Count with Differential (CBC w/diff) → To evaluate for symptoms of blood disorders such as anemia and thrombocytopenia.
The Basic Metabolic Panel (BMP) → It reveals markers for chronic kidney disease and renal failure.
Urine analysis → It might identify hemoglobinuria and hemosiderosis.
Reticulocyte count → It measures the number of immature red blood cells in bone marrow.
Haptoglobin test → Low levels might suggest damaged red blood cells.
LDH → Higher levels could suggest more red blood cell destruction.
Liver function → It monitors bilirubin levels, which could increase as red blood cells break down.
Life Expectancy of Paroxysmal Nocturnal Hemoglobinuria
Before the development of complement inhibitors like eculizumab, PNH patients typically survived between 10 and 22 years.
After the development of eculizumab and ravulizumab, the survival of PNH patients is close to that of those without the disease.
Common complications associated with PNH include thrombosis (hepatic, cerebral, and abdominal), kidney disease (acute or chronic), pulmonary hypertension, erectile dysfunction, and dysphagia.
Treatment options for Paroxysmal Nocturnal Hemoglobinuria (PNH)
Before 2000, the only available treatment for hemolytic paroxysmal nocturnal hemoglobinuria (PNH) was symptomatic therapy.
Eculizumab biosimilars have demonstrated comparable effectiveness in controlling hemolysis and associated symptoms.
The emergence of complement inhibitors (CIs) like eculizumab modified therapy strategies, leading to a 92% reduction in thromboembolic events and better survival rates.
Breakthrough hemolysis (BTH) is still problematic, and some patients may need to have their dosage intervals adjusted.
Compared to eculizumab, ravulizumab, which was approved in 2018, offers better pharmacokinetic control over C5 levels and longer dosage intervals.
In 2024, the European Medicines Agency (EMA) licensed crovalimab, which targets particular C5 epitopes, which are specific regions on the complement component C5 protein that can be recognized by antibodies, by employing innovative administration mechanisms.
Cemdisiran, an RNA interference therapy, is intended to decrease C5 synthesis in the liver, potentially helping to prevent BTH.
Ongoing clinical trials are evaluating these novel therapy techniques.
Can Paroxysmal Nocturnal Hemoglobinuria (PNH) Be Prevented?
A genetic mutation triggers PNH; therefore, it cannot be prevented.
Self-Care and Lifestyle Tips for Paroxysmal Nocturnal Hemoglobinuria (PNH)
-
- Eat a balanced diet.
- Use light exercises to manage fatigue.
- Get adequate rest and focus on stress reduction techniques like meditation or yoga.
- Stay hydrated and watch your symptoms.
- Talk with your doctor about your medications.
- Stay informed about your condition and consider joining support groups.
Summary
Allogeneic bone marrow transplants, supplemental iron, anti-thrombosis prophylaxis, and blood transfusions are considered first-line treatments.
Drugs that block alternative complement pathways, such as ravulizumab and eculizumab, as well as allogeneic hematopoietic stem cell transplantation, can also be used.
Ravulizumab is more affordable and has fewer breakthrough hemolysis attacks, while eculizumab reduces transfusion requirements and thrombotic events.
The only treatment that can treat PNH is allogeneic hematopoietic stem cell transplantation; alternate therapies target possible side effects, such as acute kidney injury, which is best managed with continuous renal replacement therapy (CRRT).
References
- Shah, N., & Bhatt, H. (2023, July 31). Paroxysmal nocturnal hemoglobinuria. In StatPearls. StatPearls Publishing. PubMed
- Panse, J. P., Höchsmann, B., & Schubert, J. (2024). Paroxysmal Nocturnal Hemoglobinuria, Pathophysiology, Diagnostics, and Treatment. Transfusion medicine and hemotherapy : offizielles Organ der Deutschen Gesellschaft fur Transfusionsmedizin und Immunhamatologie, 51(5), 310–320. Karger