Aplastic anemia (AA) is the syndrome of chronic primary hematopoietic failure caused by injury, which results in decreased or absent hematopoietic precursors in the bone...
Aplastic Anemia | Causes, Symptoms, Diagnosis and Treatments
What is Aplastic Anemia?
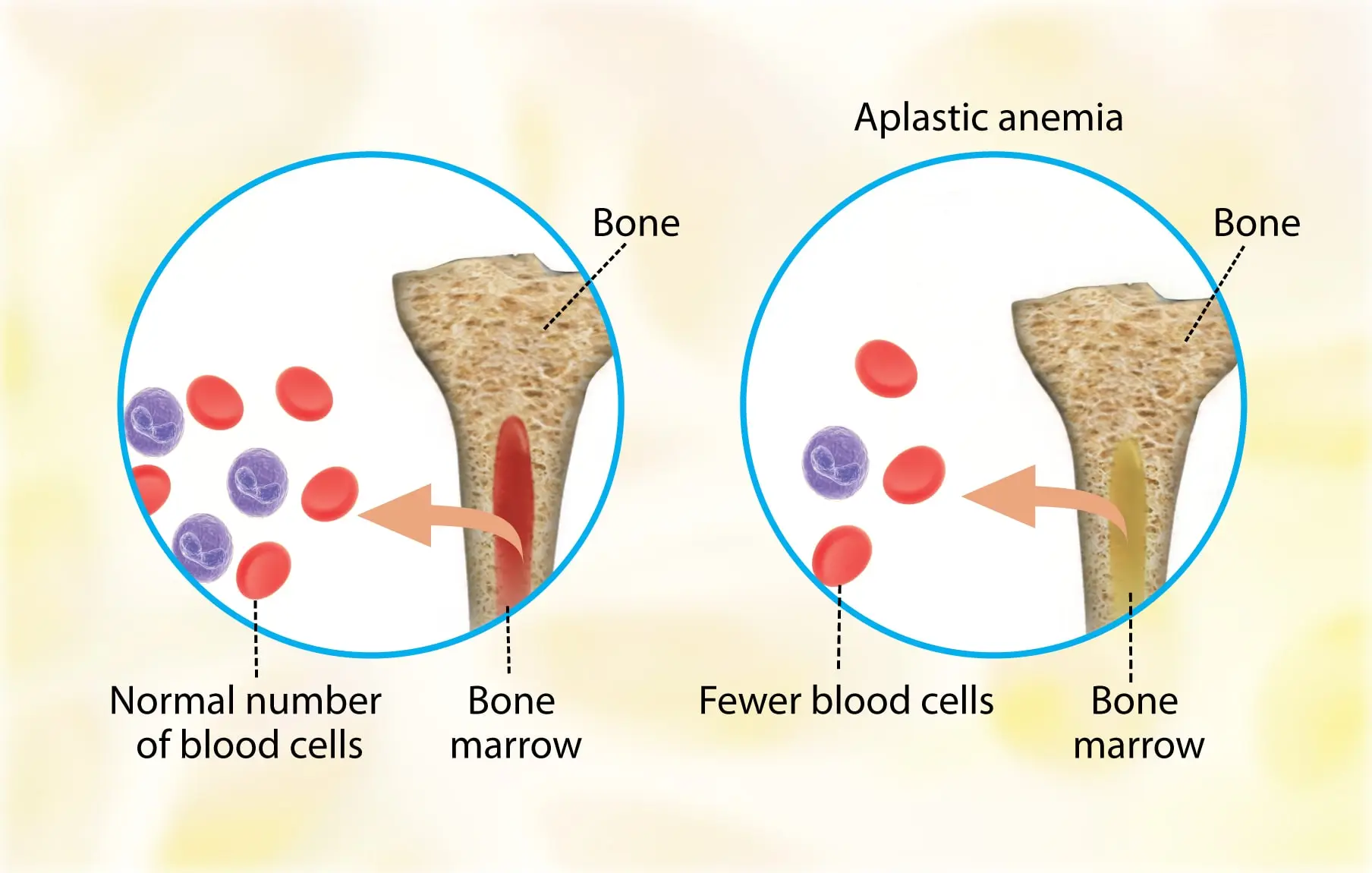
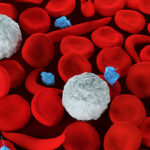
Aplastic anemia (AA) is the syndrome of chronic primary hematopoietic failure caused by injury, which results in decreased or absent hematopoietic precursors in the bone marrow and accompanying pancytopenia.
Classification of Aplastic Anemia
Aplastic anemia is classified as either moderate, severe (SAA), or very severe (vSAA).
Epidemiology of Aplastic Anemia
Aplastic anemia is a rare condition, with an annual incidence rate of 2-2.3 cases per million people.
The sex ratio is almost always near 1:1 in population-based studies.
Pathophysiology of Aplastic Anemia
Three primary mechanisms can result in the development of AA: –
- Direct injury.
- Immune-mediated.
- Inherited or acquired bone marrow failure.
1. Direct injury
As with chemotherapy and radiotherapy, bone marrow damage can be iatrogenic and dose-dependent, resulting in a predictable temporary state of reduced hematopoiesis.
Some drugs can have an atypical and possibly permanent effect, which can occur many weeks after treatment is stopped.
Hepatitis-associated AA (haAA) typically appears 2-3 months after an episode of acute hepatitis, is frequently seronegative, and accounts for up to 10% of all AA cases.
2. Immune-mediated
The majority of cases of AA have been classified as idiopathic because there is no known cause.
The dysregulated immune system appears to be centered on cytotoxic T cells, which destroy hematopoietic stem cells by: –
- Activating apoptosis via the Fas/FasL pathway (directly).
- Increasing INF-γ and TNF production (indirectly).
Some primary immunodeficiencies, such as cytotoxic T-lymphocyte associated antigen CTLA-4 and deficiency of adenosine deaminase 2 (DADA2) deficiencies, have been linked to the development of iAA as part of a complex immune dysregulation that includes autoimmunity and persistent infections with unusual organisms.
GATA2 deficiency is associated with AA as well as clonal evolution to myeloid malignancies and increased susceptibility to mycobacteria and papillomaviruses.
It also has defective hematopoietic cell differentiation and self-renewal.
3. Bone marrow failure related
Inherited bone marrow failure syndromes
Inherited bone marrow failure syndromes (IBMFS) are a group of inherited conditions that, like GATA2 deficiency, are associated with a higher risk of developing AA and clonal myeloid dysplasia.
Examples of such conditions include Fanconi anemia and dyskeratosis congenital, caused by loss-of-function germline mutations that affect the ability to repair DNA and telomeres, respectively.
Causes of Aplastic Anemia
A reduction in the number of pluripotent stem cells below a critical mass causes aplastic anemia.
This is a result of the conflict between differentiation and self-renewal.
The result is stem-cell or bone marrow failure.
Usually, AA is idiopathic, however, it can be attributable to: –
- Radiation.
- Toxic chemicals (like Benzene, solvents, and glue vapors).
- Cytotoxic drugs (chloramphenicol, gold).
- Immune-related disorders (Eosinophilic fasciitis, SLE, Graft versus host disease).
- Thymoma.
- Viral infections (Epstein-Virus Infection, Parvovirus B19, Human immunodeficiency virus (HIV), and Hepatitis virus).
- Anorexia nervosa and paroxysmal nocturnal hemoglobinuria (PNH).
Symptoms of Aplastic Anemia
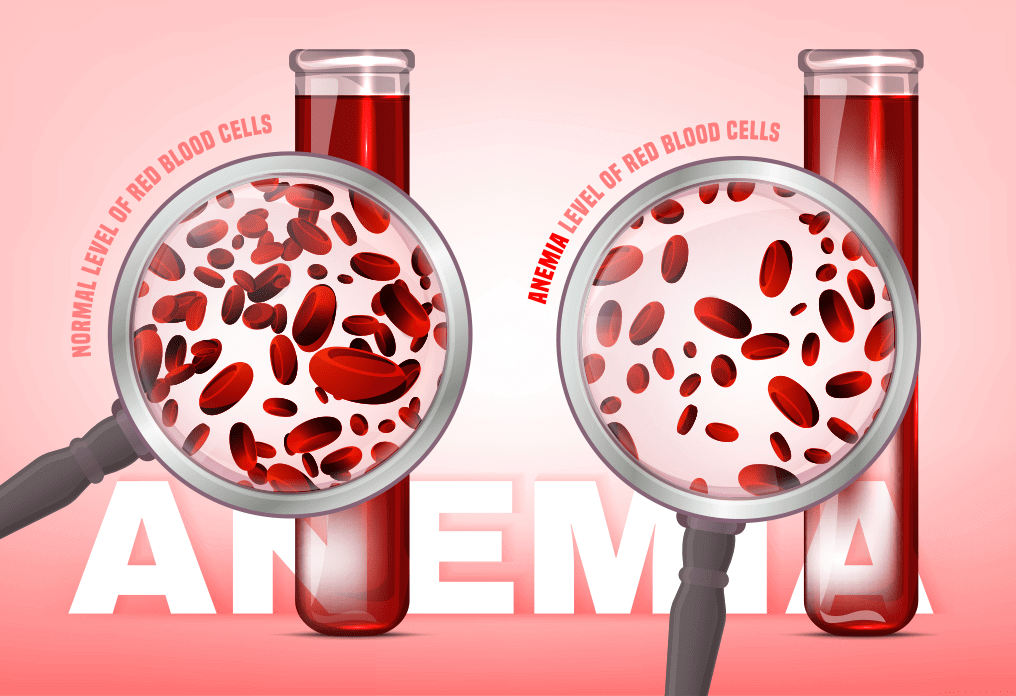
Patients typically present with non-specific symptoms caused by associated cytopenia, such as: –
- Low energy levels, pallor, and headaches with anemia.
- Mucosal bleeding.
- Bruising/petechiae.
- Menorrhagia with thrombocytopenia.
- Fever with or without evidence of infection with neutropenia.
Complications of Aplastic Anemia
The most common complications of aplastic anemia are bleeding, infections, and transformation to lymphoproliferative disorders.
These are controlled through observation and symptomatic therapy such as antibiotics, chemotherapy, and/or blood transfusions.
Diagnosis of Aplastic Anemia
Aplastic anemia has the following diagnostic criteria: –
The presence of bone marrow hypocellularity and two or more cytopenias (reticulopodia less than 1% or less than 40,000/microliter, neutropenia less than 500/microliter, or thrombocytopenia less than 20,000/microliter).
The bone marrow cellularity in moderate disease is less than 30%.
The severe disease has less than 25% cellularity or less than 50% cellularity with fewer than 30% hematopoietic cells.
Very severe meets the severe criteria in addition to neutropenia less than 200/µL.
Bone marrow aspirate has a little yield (dry tap).
It is crucial to take a bone marrow biopsy because it will be markedly hypocellular and devoid of marrow progenitors.
To rule out hematologic malignancies that cause pancytopenia, genetic testing using flow cytometry and fluorescence in situ hybridization (FISH) is useful.
Depending on the underlying cause of bone marrow failure, additional testing may be necessary, such as telomerase mutation testing for dyskeratosis congenital.
Treatment of Aplastic Anemia
Aplastic anemia treatment focuses on the underlying cause.
If possible, remove the offending agent(s).
Several medications have been stopped in the United States because of their associations with aplastic anemia (e.g., Ticlopidine, and phenylbutazone).
Most thymoma patients recover their full bone marrow after thymectomy.
Treatment is dependent on the patient’s age, disease severity, donor availability, and performance status when there is no distinctive reversible cause.
Young patients (less than 50 years old) with severe disease who are in good health should receive an allogeneic hematopoietic cell transplant (HCT) before starting immunosuppressive therapy.
Older patients (50 years and older) in good health, as well as young patients without an HCT donor, are given full-dose immunosuppressive therapy using: –
- Eltrombopag.
- Horse/rabbit anti-thymocyte globulin (ATG).
- Cyclosporine A.
- Prednisone.
For less healthy people, this combination can be tailored to include single-agent eltrombopag, ATG, or cyclosporine A.
Infection prophylaxis/treatment and transfusions are examples of supportive care.
Aplastic Anemia Life Expectancy Without Treatment
The majority of untreated patients die from disease-related complications in less than a year (e.g., bleeding, infections, or transformation to lymphoproliferative disorders).
Aplastic Anemia Life Expectancy With Treatment
Aplastic anemia survival is largely determined by age, disease severity, and response to initial therapy.
Those who recover following drug discontinuation or treatment of the underlying condition, as well as those with self-limited processes, have a stable clinical course.
Patients who receive a bone marrow transplant from a suitable donor have a five-year survival rate of more than 75%.
Summary
Aplastic anemia (AA) is the syndrome of chronic primary hematopoietic failure caused by injury, which results in decreased or absent hematopoietic precursors in the bone marrow and accompanying pancytopenia.
Aplastic anemia is classified as either moderate, severe (SAA), or very severe (vSAA).
Three primary mechanisms can result in the development of AA: –
- Direct injury.
- Immune-mediated.
- Inherited or acquired bone marrow failure.
Usually, AA is idiopathic, however, it can be attributable to: –
- Radiation.
- Toxic chemicals (like Benzene, solvents, and glue vapors).
- Cytotoxic drugs (chloramphenicol, gold).
- Immune-related disorders (Eosinophilic fasciitis, SLE, Graft versus host disease).
- Thymoma.
- Viral infections (Epstein-Virus Infection, Parvovirus B19, Human immunodeficiency virus (HIV), and Hepatitis virus).
- Anorexia nervosa and paroxysmal nocturnal hemoglobinuria (PNH).
Patients typically present with non-specific symptoms caused by associated cytopenia, such as: –
- Low energy levels, pallor, and headaches with anemia.
- Mucosal bleeding.
- Bruising/petechiae.
- Menorrhagia with thrombocytopenia.
- Fever with or without evidence of infection with neutropenia.
The most common complications of aplastic anemia are bleeding, infections, and transformation to lymphoproliferative disorders.
Aplastic anemia has the following diagnostic criteria: –
The presence of bone marrow hypocellularity and two or more cytopenias (reticulopodia less than 1% or less than 40,000/microliter, neutropenia less than 500/microliter, or thrombocytopenia less than 20,000/microliter).
The bone marrow cellularity in moderate disease is less than 30%.
The severe disease has less than 25% cellularity or less than 50% cellularity with fewer than 30% hematopoietic cells.
Very severe meets the severe criteria in addition to neutropenia less than 200/µL.
Aplastic anemia treatment focuses on the underlying cause.
If possible, remove the offending agent(s).
Treatment is dependent on the patient’s age, disease severity, donor availability, and performance status when there is no distinctive reversible cause.
Young patients (less than 50 years old) with severe disease who are in good health should receive an allogeneic hematopoietic cell transplant (HCT) before starting immunosuppressive therapy.
Older patients (50 years and older) in good health, as well as young patients without an HCT donor, are given full-dose immunosuppressive therapy using: –
- Eltrombopag.
- Horse/rabbit anti-thymocyte globulin (ATG).
- Cyclosporine A.
- Prednisone.
How useful was this post?
Click on a star to rate it!
Average rating 0 / 5. Vote count: 0
No votes so far! Be the first to rate this post.
I'm sorry that this post was not useful for you!
Let me improve this post!
Tell me how I can improve this post?
References
- Aplastic anemia – statpearls – NCBI bookshelf. Retrieved March 17, 2023, from PubMed
- (PDF) aplastic anemia- A quick review – researchgate. Retrieved March 17, 2023, from ResearchGate
Aplastic anaemia: Current concepts in diagnosis and management – wiley online library. Retrieved March 17, 2023, from Wiley Online Library
Macrocytic anemia is defined as macrocytosis (mean corpuscular volume (MCV) greater than 100 fL). Macrocytosis affects 2% to 4% of the population, 60% of whom...
People who abuse alcohol are typically at risk for a wide range of alcohol-related medical complications. Alcohol has a variety of negative effects on blood...
Anemia of chronic disease, also known as anemia of chronic inflammation, is caused primarily by infections, autoimmune disorders, chronic renal insufficiency, and malignancies.
Featured Posts
Recent Posts
Popular Posts
Learn More