Acute Pancreatitis (AP) is an acute pancreatic inflammatory disorder caused by intracellular activation of pancreatic digestive enzymes.
Gastric Ulcers | Causes, Symptoms, Complications & Treatments
Introduction
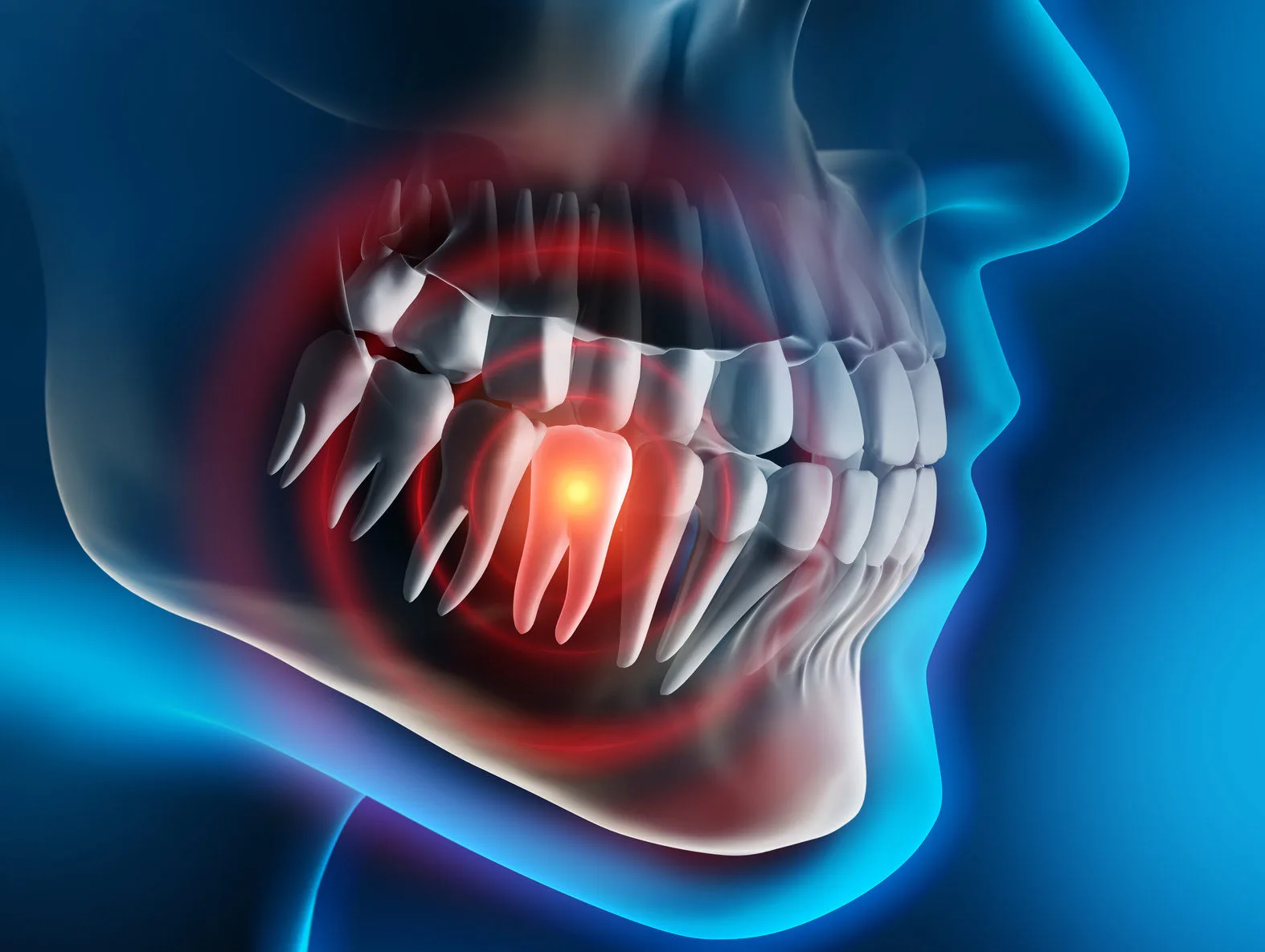
Gastric ulcers are defined as a break in the mucosal barrier of the stomach lining that penetrates through the muscularis mucosa and is larger than 5 mm in diameter.
They are a common clinical presentation in the United States and frequently result in the expenditure of millions of dollars in healthcare.
The body has a natural way of protecting the gastric mucosa from the harmful acidic environment which is called the gastric lumen.
Alterations in these defenses can cause changes in the gastric mucosa, eventually leading to erosions and ulcers.
The gastric mucosa is protected by prostaglandins, mucus, growth factors, and adequate blood flow.
Known factors that can damage this barrier include smoking, hydrochloric acid, ischemia, NSAID medications, hypoxia, alcohol, and Helicobacter pylori infection.
It is important to understand that this disease process is both preventable and treatable.
Treatment may vary depending on the cause of the gastric ulcer.
Pathophysiology of Gastric Ulcers
The pathophysiology of gastric ulcers depends on their cause.
Helicobacter pylori and/or NSAID use cause 80-90 % of gastric ulcers.
A. Helicobacter Pylori
These bacteria colonies are 45-50% of the stomach mucosa worldwide.
The bacteria are inoculated at an early age, especially in developing countries with low socioeconomic status and crowded households.
These bacteria induce an inflammatory response in the host, causing an epithelial reaction, degeneration, and injury known as gastritis.
Patients who have this infection typically develop pan-gastritis.
This damages antral somatostatin release, resulting in increased gastrin secretion which stimulates increased acid production.
Patients who develop gastric ulcers are those in whom the bacteria remain in the antrum.
CagA production is a common bacterial virulence factor that leads to more cytokine cell destruction and mucosal damage.
B. NSAIDs Use
NSAIDs are the second most common cause of gastric ulcers.
Patients taking these drugs have a relative risk of four times higher than those not taking them for gastric ulcers.
There are multiple mechanisms by which NSAIDs cause ulcers.
The drugs themselves are weak acids when they become exposed to gastric acid.
It remains in the epithelial cells, causing increased cell permeability, are leading to physical cell injury.
The primary mechanism of NSAID-induced ulcer formation is decreased prostaglandin synthesis.
Causes of Gastric Ulcers
The common factor in all of these causes is that they promote a breakdown in the mucosal barrier, exposing the gastric mucosa to the damaging effects of acid.
The most common causes of gastric ulcers include: –
- Bacterial infection with Helicobacter pylori.
- Gastric prostaglandin loss associated with NSAID drugs.
Less common causes include: –
- Hypergastrinemia (Zollinger-Ellison syndrome).
- CMV and other viral infections.
- Chemotherapy and radiation therapy.
- Gastric outlet obstruction.
- Gastric invasive disease such as malignancy.
- Cigarette smoking.
- Crohn’s disease.
Symptoms of Gastric Ulcers
- Bloating and abdominal distention.
- Nausea and profuse vomiting.
- Melena.
- Chest pain.
- Hematemesis.
- Anorexia and weight loss.
- Abdominal and epigastric pain related to meal time.
- Perforation of the stomach or duodenum resulting in acute peritonitis.
Complications of Gastric Ulcers
The following are the most common gastric ulcer complications: –
- Gastrointestinal (GI) bleeding.
- Gastric perforation (GI perforation).
- Gastric penetration.
- Gastric outlet obstruction.
Treatment of Gastric Ulcers
The goal of treatment and management of gastric ulcers is first to elevate the pH of the stomach and allow the gastric mucosa to heal.
This can be done by administering a proton pump inhibitor such as pantoprazole.
The next step should be to decide whether to proceed with an EGD.
These patients must receive PPI therapy twice daily for 8 weeks before having another endoscopy to verify healing.
If an NSAID is being used, it should be discontinued immediately.
If Helicobacter pylori infection is detected through biopsies or laboratory testing, antibiotic therapy is necessary to treat the condition, and eradication must also be confirmed.
If the gastric ulcer is bleeding, an epinephrine injection with cautery or metal or absorbable clip placement is usually effective.
In cases where endoscopic therapy is ineffective or not recommended, surgical management may be required.
Indications for surgical intervention include uncontrolled bleeding, perforation, severe gastric outlet obstruction, and ulcers that do not heal with medical therapy.
Summary
Gastric ulcers are defined as a break in the mucosal barrier of the stomach lining that penetrates through the muscularis mucosa and is larger than 5 mm in diameter.
They are a common clinical presentation in the United States and frequently result in the expenditure of millions of dollars in healthcare.
The body has a natural way of protecting the gastric mucosa from the harmful acidic environment which is called the gastric lumen.
The pathophysiology of gastric ulcers depends on their cause.
Helicobacter pylori and/or NSAID use cause 80-90 % of gastric ulcers.
The common factor in all of these causes is that they promote a breakdown in the mucosal barrier, exposing the gastric mucosa to the damaging effects of acid.
The most common causes of gastric ulcers include: –
- Bacterial infection with Helicobacter pylori.
- Gastric prostaglandin loss associated with NSAID drugs.
The goal of treatment and management of gastric ulcers is first to elevate the pH of the stomach and allow the gastric mucosa to heal.
This can be done by administering a proton pump inhibitor such as pantoprazole.
The next step should be to decide whether to proceed with an EGD.
These patients must receive PPI therapy twice daily for 8 weeks before having another endoscopy to verify healing.
If an NSAID is being used, it should be discontinued immediately.
If Helicobacter pylori infection is detected through biopsies or laboratory testing, antibiotic therapy is necessary to treat the condition, and eradication must also be confirmed.
How useful was this post?
Click on a star to rate it!
Average rating 0 / 5. Vote count: 0
No votes so far! Be the first to rate this post.
I'm sorry that this post was not useful for you!
Let me improve this post!
Tell me how I can improve this post?
References
- Woolf, Andrew, and Robert Rose. “Gastric Ulcer.” Nih.gov, StatPearls Publishing, 28 Jan. 2019, From PubMed.
Francesco Di Mario, et al. Short-Term Treatment of Gastric Ulcer. Vol. 41, no. 6, 1 June 1996, pp. 1108–1131, From Link Springer.
Gastric Ulcers | Causes, Symptoms, Complications & Treatments
Gastric ulcers are defined as a break in the mucosal barrier of the stomach lining that penetrates through the muscularis mucosa and is larger than...
Featured Posts
Recent Posts
Popular Posts
Learn More