Acute Pancreatitis (AP) is an acute pancreatic inflammatory disorder caused by intracellular activation of pancreatic digestive enzymes.
Acute Pancreatitis | Causes, Symptoms, Diagnosis and Treatments
Introduction
Acute Pancreatitis (AP) is an acute pancreatic inflammatory disorder caused by intracellular activation of pancreatic digestive enzymes.
It is considered one of the most common gastrointestinal diseases, resulting in a significant emotional, physical, and financial human burden, as well as high morbidity and mortality.
The severity of acute pancreatitis ranges from mild conditions requiring conservative treatment to severe and complicated diseases with high morbidity and mortality.
Causes of Acute Pancreatitis
The most common causes of acute pancreatitis are hypertriglyceridemia, alcohol use, and gallstones.
Here is a list of Common causes of acute pancreatitis
- Gallstones.
- Alcohol use.
- Hypertriglyceridemia.
- Drug-induced pancreatitis.
- Smoking.
- Trauma.
- Hypercalcemia.
- Autoimmune pancreatitis, type I and type II.
- Renal disease (Hemodialysis).
- Post-procedural, e.g., abdominal surgery.
- Ampullary stenosis, which is formerly known as sphincter of Oddi dysfunction type I.
- Toxins (Scorpion bites, organophosphate poisoning).
- Viral infections i.e., Cytomegalovirus, Hepatitis A/B/C, and HIV.
- Bacterial infections i.e., Legionella and Mycobacterium tuberculosis.
- Post-procedural, e.g., abdominal surgery.
- Congenital anomalies, e.g., annular pancreas
- Genetic disorders like hereditary pancreatitis.
- Parasitic infections i.e., Ascaris lumbricoides, and Clonorchis Sinensis.
- Vasculitis i.e., Systemic lupus erythematosus.
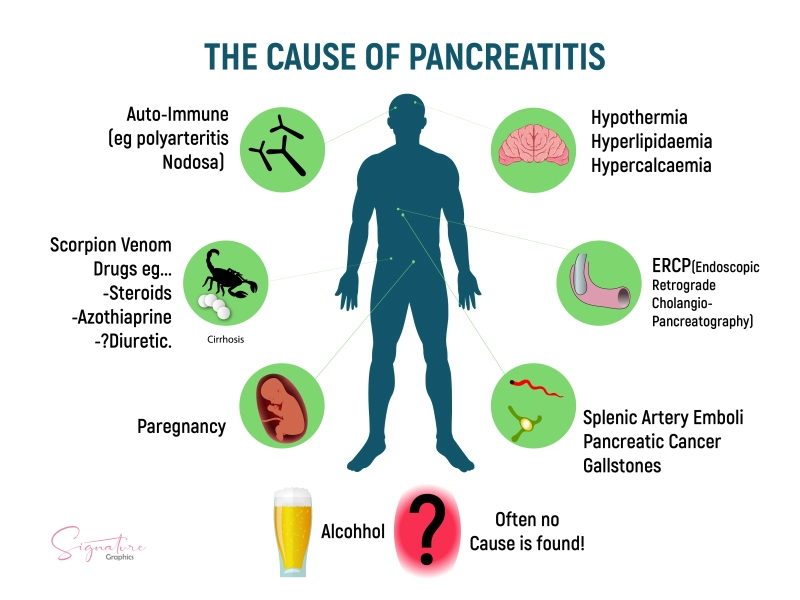
Causes of Pancreatitis
Signs & Symptoms of Acute Pancreatitis
Acute pancreatitis typically manifests as upper abdominal pain, nausea, vomiting, and fever. (Abdominal pain is the major symptom).
A physical examination is frequently important for identifying fever, tachycardia, and in severe patients, hypotension.
The abdominal exam will typically reveal epigastric tenderness, as well as possible guarding, rigidity, and decreased bowel sounds.
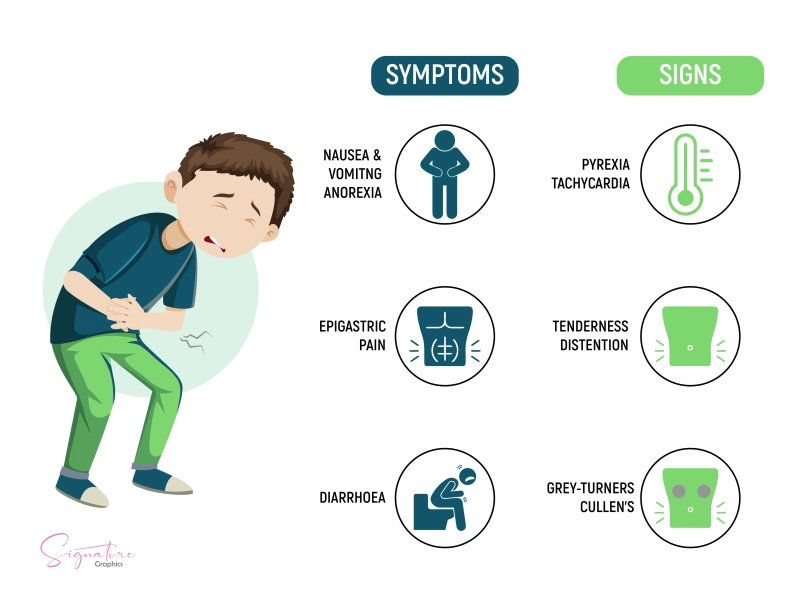
Signs and Symptoms of Pancreatitis
Types of Acute Pancreatitis
Acute pancreatitis is classified into three types based on its severity: –
Mild acute pancreatitis à The most common form and has no organ failure, or local or systemic complications, and usually resolves within a week.
Moderately severe acute pancreatitis à It is identified by the presence of transient organ failure, local complications, or exacerbation of co-morbid disease.
Severe acute pancreatitis à It is characterized by persistent organ failure lasting more than 48 hours and involving one or more organs.
Complications of Acute Pancreatitis
- Abdominal compartment syndrome.
- Gastric varices.
- Acidosis.
- Acute renal failure.
- Mesenteric venous thrombosis
- Acute respiratory distress syndrome.
- Pancreatic abscess.
- Ascites.
- Pancreatic arterial pseudoaneurysm.
- Bowel infarction.
- Pancreatic necrosis.
- Chronic pancreatitis.
- Pseudocyst formation.
- Disseminated intravascular coagulation.
- Splenic venous thrombosis.
- Hemorrhagic pancreatitis.
Diagnosis of Acute Pancreatitis
Acute pancreatitis is diagnosed using magnetic resonance cholangiopancreatography (MRCP), computed tomography (CT), and ultrasonography (US) as well as blood tests to measure serum lipase and amylase levels.
Although measurements of serum and urinary enzymes are used to diagnose AP, none of them allow for a precise evaluation of the disease’s severity or prediction of how it will manifest clinically.
Ultrasonography is recommended as a first and basic imaging test in patients with suspected AP to confirm or exclude the diagnosis and to detect the possible cause of the disease.
In moderate to severe cases, a chest radiograph is usually performed to check for pleural effusions, which indicate a higher severity of the disease and a higher mortality rate.
When the diagnosis is unclear but pancreatitis is suspected, computed tomography (CT) with intravenous contrast is recommended to establish or rule out the diagnosis.
MRI and CT help identify pancreatic necrosis, diagnose local complications, and assess the severity of AP.
Treatment of Acute Pancreatitis
Acute pancreatitis is a self-limiting condition that usually resolves on its own within 3 to 7 days in the majority of patients (85–90%).
Conventional measures include: –
- Analgesics.
- Intravenous fluids and colloids to maintain normal intravascular volume.
- No oral alimentation.
- Elective nasogastric suction decreases gastrin release from the stomach and prevents gastric contents from entering the duodenum.
A clear liquid diet can usually be started on the third to the sixth day, and a regular diet on the fifth to the seventh day.
A patient with severe pancreatitis requires the diagnostic, therapeutic, and nursing advantages of an intensive care unit, as well as close attention to complications.
Preventing infection is essential because the development of infected necrosis significantly increases mortality in patients with acute necrotizing pancreatitis.
The prophylactic antibiotic of choice in radiographically proven necrosis is imipenem-Cilastatin.
It should be continued for at least two to four weeks.
The treatment of necrosis has shifted from early surgical debridement to aggressive intensive medical care with specific criteria for operative and nonoperative intervention.
Summary
Acute Pancreatitis (AP) is an acute pancreatic inflammatory disorder caused by intracellular activation of pancreatic digestive enzymes.
It is considered one of the most common gastrointestinal diseases, resulting in a significant emotional, physical, and financial human burden, as well as high morbidity and mortality.
The most common causes of acute pancreatitis are hypertriglyceridemia, alcohol use, and gallstones.
AP typically manifests as upper abdominal pain, nausea, vomiting, and fever. (Abdominal pain is the major symptom).
It is classified into three types based on its severity: –
- Mild acute pancreatitis.
- Moderately severe acute pancreatitis.
- Severe acute pancreatitis.
AP is diagnosed using magnetic resonance cholangiopancreatography (MRCP), computed tomography (CT), and ultrasonography (US) as well as blood tests to measure serum lipase and amylase levels.
It is a self-limiting condition that usually resolves on its own within 3 to 7 days in the majority of patients (85–90%).
Conventional measures include: –
- Analgesics.
- Intravenous fluids and colloids to maintain normal intravascular volume.
- No oral alimentation.
- Elective nasogastric suction decreases gastrin release from the stomach and prevents gastric contents from entering the duodenum.
How useful was this post?
Click on a star to rate it!
Average rating 0 / 5. Vote count: 0
No votes so far! Be the first to rate this post.
I'm sorry that this post was not useful for you!
Let me improve this post!
Tell me how I can improve this post?
References
- (PDF) acute pancreatitis – researchgate. ResearchGate
- Acute pancreatitis – statpearls – NCBI bookshelf. PubMed
- S;, G. J. A. Acute pancreatitis. National Center for Biotechnology Information. PubMed
- Banks PA;Bollen TL;Dervenis C;Gooszen HG;Johnson CD;Sarr MG;Tsiotos GG;Vege SS; ; (n.d.). Classification of acute pancreatitis–2012: Revision of the atlanta classification and definitions by International Consensus. Gut. PubMed
- Diagnosis and treatment of acute pancreatitis – researchgate. ResearchGate
- Acute pancreatitis – researchgate. ResearchGate
(PDF) acute pancreatitis: Review article – Researchgate. ResearchGate
Gastric Ulcers | Causes, Symptoms, Complications & Treatments
Gastric ulcers are defined as a break in the mucosal barrier of the stomach lining that penetrates through the muscularis mucosa and is larger than...
Featured Posts
Recent Posts
Popular Posts
Learn More