SLE is a multisystem condition with a variety of presenting forms. The disease might range from a serious, possibly fatal condition that only affects the mucosal membrane to a relatively mild condition that affects several organs. In this article we will focus on early signs of lupus in females and possible associated risk factors.
Every organ system may be negatively affected by SLE. Autoantibody analysis can sometimes be utilized for predicting the course of the disease and its clinical symptoms.
Multiple studies have demonstrated that serological abnormalities start appearing several years prior to the onset of symptoms associated with lupus.
The risk of SLE is 14 times higher in Klinefelter syndrome and ten times higher in women than in men (47, XXY). This implies a relationship with X chromosome genes. Nevertheless, the precise genes remain unknown despite numerous investigations.
The Most Common Early Signs of Lupus in Females
The most common symptoms of newly diagnosed or recurrent active flare-ups of SLE are nonspecific fatigue, fever, arthralgia, and weight fluctuations.
Patients with SLE may have a variety of systemic symptoms. Typical first signs include fever, malaise, arthralgias, myalgias, headache, loss of appetite, and weight loss.

Uncommon Lupus Symptoms
A list of 6 rare SLE manifestations can be found which include: gastrointestinal, liver, pulmonary, cardiac, ocular and neurological manifestations.
The frequency of symptoms related to digestive tract disorders ranged from 0.5% to 10.7% of the patients; hepatitis associated to lupus (9.3%) and autoimmune hepatitis (2.3%); liver involvement was observed in many cases.
The rarest pulmonary signs observed were shrinking lung syndrome, documented in 1.5% of patients, whereas interstitial lung disease and lupus pneumonia were reported in 4% and 3% of patients respectively.
Depending on the methods employed for identification in multiple studies, myocarditis and pulmonary hypertension were also rarely seen in SLE patients, with reported rates ranging from 0.4-16% and 1-14%, respectively.
Rare symptoms (reported in less than 5% of patients) and lupus retinopathy (documented in 1.2–28.8% of patients, depending on techniques of identification) are among the ocular signs of SLE.
It was also found that aseptic meningitis and chorea were extremely uncommon symptoms, occurring in less than 1% and 0.3-2.4% of patients, respectively.
Risk Factors for Lupus in Women
The following risk factors could be responsible for early signs of lupus in females.
Hormonal factors and female sex are important risk factors for SLE.
Thymocytes, B cells, CD8+ and CD4+ T cells, macrophages, and the production of certain cytokines (including IL-1) are all stimulated by estrogen.
It also causes the expression of HLA and endothelial cell adhesion molecules (VCAM, ICAM).
Furthermore, B-cell activation factor synthesis is increased, lymphocyte and plasmacytoid dendritic cell (pDC) activation are modulated, and autoimmunity is encouraged by estrogens and prolactin.
In addition to being linked to a higher incidence of SLE, the use of postmenopausal hormonal replacement therapy and estrogen-containing contraception can trigger flare-ups in SLE patients.
Furthermore, prolactin levels are higher in SLE patients. Conversely, androgens depress the immune system.
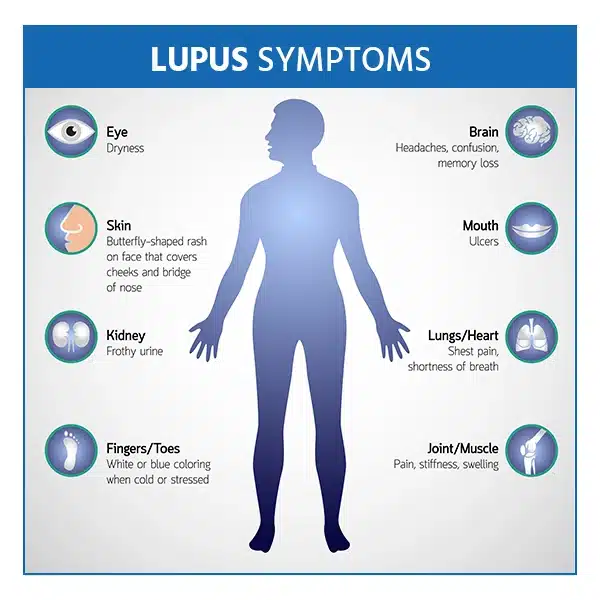
Lupus Symptoms in Women
Among the most typical symptoms of lupus in women are provided in the following table
- Rashes elsewhere on the body or a butterfly-shaped rash covering the cheeks and nasal bridge
- Skin sores that develop or get worse when exposed to sunlight
- Feeling tired
- High temperatures
- Aching, rigid, and swollen joints
- Fingers and toes that turn blue or white in the presence of cold weather or during times of stress
- Chest discomfort
- Eye dryness
- Headaches, confusion, and amnesia
- Difficulty breathing
Expectations during Early and Dying Stages of Lupus
Studies genuinely show that the main causes of death in the early phases of the illness are infection and disease activity, particularly if it involves the kidneys and central nervous system.
End-stage lupus symptoms are particular to the complication or afflicted organ or system. The most common complications that cause death are cardiovascular disease, kidney failure, and malignancy.
Cardiovascular diseases responsible for the vast majority over time.
Can Lupus Kill you?
The all-cause mortality rate among SLE patients is 2.6 times higher than that of the general population.
Patients who are 44 years of age or younger are particularly at risk for all-cause mortality, with a 5.5-fold greater likelihood of dying.
Cardiovascular illnesses and cancer were the most frequent causes of death in most of cases, although infectious diseases accounted for a proportion of deaths lower than that previously reported.
Summary
Early signs of lupus in females should detected as soon as possible and rapid diagnosis and management should be implemented.
These symptoms, such as fever, skin rashes, joint pain, and chronic exhaustion, can prevent complications and organ damage, enhancing patients’ quality of life and long-term prognosis.
[ratemypost]
References
- Cojocaru, M., Cojocaru, I. M., Silosi, I., & Vrabie, C. D. (2011). Manifestations of systemic lupus erythematosus. Maedica (Bucur), 6(4), 330-336. From PubMed.
- Tani, C., Elefante, E., Arnaud, L., et al. (2022). Rare clinical manifestations in systemic lupus erythematosus: A review on frequency and clinical presentation. Clinical and Experimental Rheumatology, 40 (Suppl 134), 93-102. From PubMed.
- Justiz Vaillant, A. A., Goyal, A., & Varacallo, M. (2023). Systemic lupus erythematosus. In StatPearls [Internet]. Treasure Island (FL): Stat Pearls Publishing. Retrieved from PubMed.
- Reis-Neto, E. T. dos, Monticielo, O. A., Daher, M., Lopes, F., Angrimani, D., & Klumb, E. M. (2024). Life expectancy and death pattern associated with systemic lupus erythematosus diagnosis in Brazil between 2000 and 2019. Lupus, 33(5), 536-542. From PubMed.
- Zen, M., Salmaso, L., Barbiellini Amidei, C., et al. (2023). Mortality and causes of death in systemic lupus erythematosus over the last decade: Data from a large population-based study. From PubMed.