Firstly, before discussing pancreatitis and when to worry, it is essential to understand what it is.
Pancreatitis is an inflammatory condition of the pancreas caused by the activation and retention of digestive enzymes.
Types of pancreatitis, as well as their causes, and symptoms will be discussed in this article.
Just continue reading to learn when pancreatitis necessitates immediate attention!
Pancreatitis: When to Worry?
The pancreas is an exocrine and endocrine gland located beneath the stomach, close to the duodenum.
It is responsible for managing the following functions:
- The exocrine portion secretes digestive enzymes on a daily basis, which aid in the digestion of fats, proteins, and carbohydrates.
- The endocrine section regulates glucose levels by secreting hormones like insulin and glucagon.
Pancreatitis is a dangerous state marked by inflammation, which includes swelling, redness, warmth, and pain.
Can You Die From Pancreatitis?
Yes, you can die from pancreatitis according to its types, as pancreatitis is classified into acute and chronic.
Acute pancreatitis is a rapid inflammatory condition that can range from mild to severe.
Thus, it can cause life-threatening complications often resulting in:
- Necrosis
- Sepsis
- Organ failure in the lungs, kidneys, heart
- Bleeding in pancreas
Chronic pancreatitis, which develops gradually over time, can lead to serious complications involving:
- Pancreatic insufficiency is when the pancreas loses its ability to secrete hormones and enzymes.
- Pancreatic cancer
- Diabetes that is caused by inadequate insulin production
- Pancreatic pseudocysts
- Malnutrition because of malabsorption of nutrients in the digestive tract
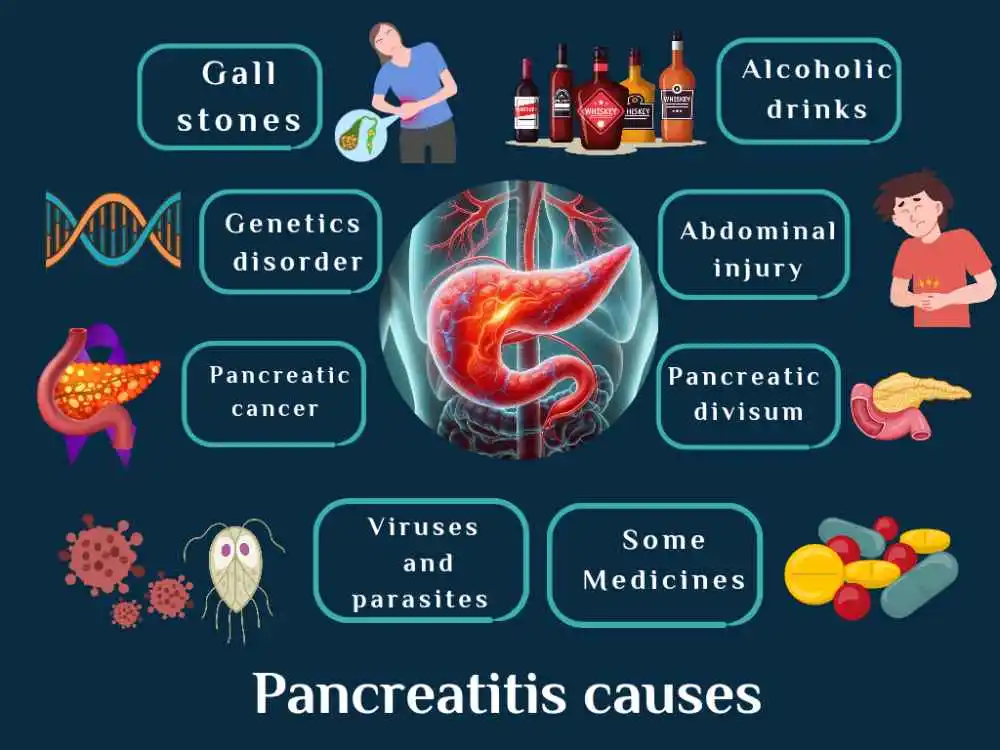
Causes Of Pancreatitis
Acute or chronic pancreatitis can be caused by a variety of reasons, which include:
- Gallstones
- Drinking alcohol heavily
- Genetic disorders
- Infection with viruses or parasites
- Pancreatic cancer
- Abdominal injury
- Pancreatic divisum: a birth abnormality in which the pancreatic sections do not fuse.
- Some medicines
- High triglyceride and calcium levels
- Obesity
- Smoking
Additionally, when doctors are unable to determine the cause of pancreatitis, idiopathic pancreatitis develops.
Pancreatitis Death Symptoms
Back pain radiating from the upper abdomen is a common symptom of both acute and chronic pancreatitis.
Nonetheless, the specific type of pancreatitis and the severity of inflammation affect the following symptoms:
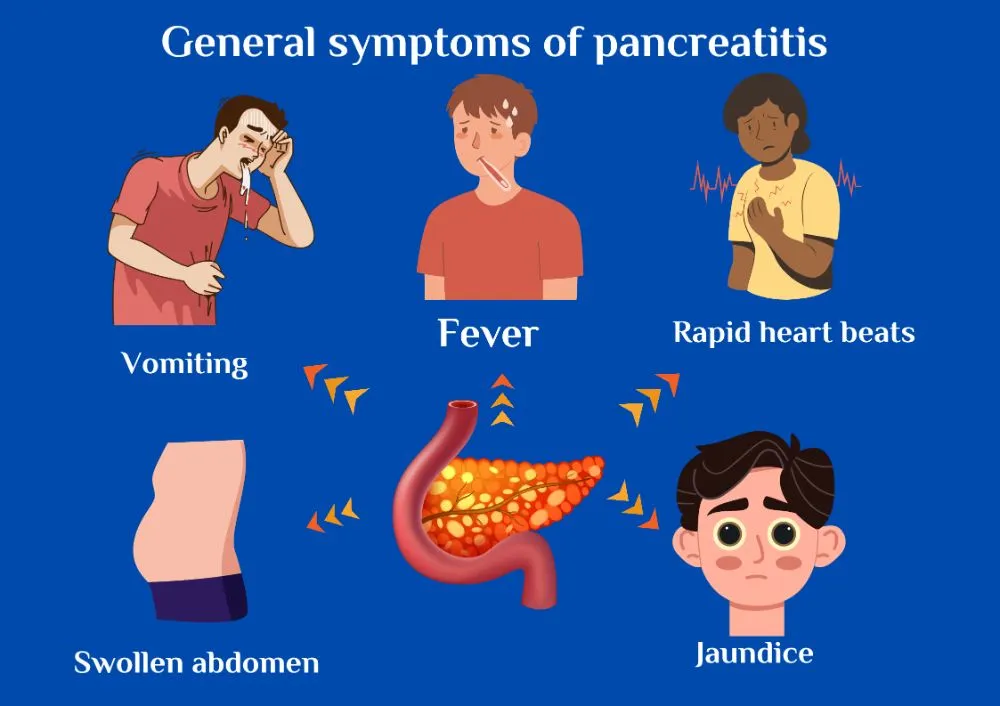
Symptoms of Acute Pancreatitis
- Vomiting and nausea
- Dehydration
- Fever and chills
- Rapid heart beats
- Swollen abdomen
- jaundice
If acute pancreatitis symptoms are left untreated, they can develop into necrotizing pancreatitis, a serious condition that can lead to pancreatic death, sepsis, and shock, threatening life by decreasing blood flow to other organs.
Chronic Pancreatitis Symptoms
Diarrhea, vomiting, nausea, weight loss, and foul-smelling feces are common symptoms of chronic pancreatitis, which often go undetected until complications emerge.
Female Pancreatitis Pain Location
Pancreatitis causes abdominal pain, which varies according to the cause.
For example, gallstone pancreatitis causes sudden, severe pain, while alcoholic pancreatitis develops slowly.
Usually, female pancreatitis causes pain in the upper abdomen, just below the ribs.
The pain may worsen after a meal or while sleeping on your back, and may persist for a few days before becoming severe and permanent.
How to Diagnose Pancreatitis?
A healthcare provider can diagnose pancreatitis through,
- Examine your abdomen for swallowing and pain.
- Examine your medical history to determine whether you have any diseases that could increase your risk of pancreatitis.
In addition, your physician uses the following lab and imaging test results to diagnose pancreatitis:
Lab tests
Acute pancreatitis is indicated by the following:
- Elevated blood levels of lipase and amylase enzymes.
- The level of blood glucose rises.
- High amounts of triglycerides.
- A fecal fat test determines whether the stool contains more fat than normal, indicating malabsorption.
Imaging tests
- A computed tomography, or (CT) scan, is used to diagnose pancreatitis.
- Ultrasounds: This instrument utilizes sound waves to identify gallstones and to create visuals of the structure of your organs.
- Meganti resonance cholangiopancreatography (MRCP) finds the etiology of pancreatitis by creating images involving bile, pancreatic ducts, and soft tissues.
- Endoscopic ultrasonography is a method that extends from the throat to the small intestine and uses a probe to discover gallstones.
Can Pancreatitis Be Cured?
For either acute or chronic pancreatitis, treatment options include:
- To treat dehydration, stay at the hospital and get intravenous fluids.
- Pancreatic infections require antibiotics and pain medications, which can be administered either intravenously or orally.
- A low-fat diet is given intravenously or through a feeding tube if you are unable to eat.
If severe acute pancreatitis is caused by gallstones, your doctor may recommend surgically removing the gallbladder to prevent complications.
Chronic pancreatitis treatment involves medications and vitamins to
- Relieve pain.
- Improve pancreatic function.
- Manage complications.
- Check up for regulation of blood glucose levels.
To enhance pancreatic functions, the surgeon suggests removing damaged and infected pancreatic sections surgically.
If not enhanced, surgery may involve removing the entire pancreas and islet autotransplantation.
Lastly, doctors counsel patients suffering from both types of pancreatitis to
- Avoid drinking alcohol.
- Stop smoking.
- Maintain a healthy lifestyle.
- Eat rich food with minerals and vitamins.
- Lose weight safely.
Summary
Pancreatitis is a serious issue that causes inflammation due to the accumulation of pancreatic enzymes and it can be acute or chronic.
Gallstones, alcohol consumption, genetic problems, infections, and certain medications can all cause acute or chronic pancreatitis.
Symptoms Of acute pancreatitis include vomiting, fever, and jaundice. Chronic pancreatitis is characterized by diarrhea, weight loss, and foul odor.
Diagnosis involves abdominal examination, medical conditions, and lab tests.
Treatment options include hospital stays, antibiotics, pain medication, a low-fat diet, and surgery in some cases.
Recommendations involve changing lifestyle, stopping smoking, and drinking alcohol.
References
- U.S. Department of Health and Human Services. (n.d.-b). Symptoms & causes of pancreatitis – NIDDK. National Institute of Diabetes and Digestive and Kidney Diseases.From NIH
- U.S. National Library of Medicine. (2021, May 25). Overview: Acute pancreatitis. InformedHealth.org [Internet]. From NIH
- Pancreatitis. Pancreatitis | Columbia Surgery. (n.d.-a). From Columbia Surgery
- U.S. Department of Health and Human Services. (n.d.-c). Treatment for pancreatitis – NIDDK. National Institute of Diabetes and Digestive and Kidney Diseases. From NIH
- Stoppacher, R. (2018, June). Sudden death due to acute pancreatitis. Academic forensic pathology. From PubMed
- U.S. Department of Health and Human Services. (n.d.-a). Diagnosis of pancreatitis – NIDDK. National Institute of Diabetes and Digestive and Kidney Diseases. From NIH
- Author links open overlay panelMarko Murruste a b, a, b, c, AbstractBackground/ObjectivesChronic pancreatitis (CP) is a complex disease with a high complications rate, Whitcomb, D. C., Majumder, S., Lankisch, P. G., Nojgaard, C., Pedrazzoli, S., Kempeneers, M. A., Charlson, M. E., Bobashev, G. V., Sohn, T. A., Ockenga, J., Sand, J., Roberts, K. J., Johnson, C. D., Warshaw, A. L., … Conwell, D. L. (2021a, March 10). Long-term survival, risk factors and causes of mortality in surgically treated chronic pancreatitis. Pancreatology. From Science Direct