Rheumatoid arthritis is a progressive, chronic, and degenerative autoimmune inflammatory disease that is primarily characterized by synovitis.
It is a chronic systemic inflammatory disorder marked by inflammation of the surrounding tissues, including tendons, ligaments, and muscles, as well as deformity of the synovial joints.
It usually begins in small peripheral joints and progresses to involve proximal joints if left untreated.
Joint inflammation leads to joint destruction over time, with cartilage loss and bone erosions.
Pathophysiology of Rheumatoid Arthritis
In RA, the immune and inflammatory systems play a crucial role in the destruction of bone and cartilage.
Rheumatoid factor (RF) and anti-citrullinated protein antibodies (ACPAs) are produced in RA and are targeted against autoantigens that are commonly found within and outside of synovial joints.
RF is produced by B cells in the synovial membrane and is linked with more aggressive joint degeneration.
RA is divided into several disease subtypes, each with its own set of inflammatory cascades that result in persistent synovial inflammation and damage to articular cartilage and underlying bone.
Tumor necrosis factor alpha (TNF-α) and interleukins 1 and 6 (IL-1, IL-6) are key inflammatory cytokines in its pathogenesis, resulting in the production of proteolytic enzymes and the activation of osteoclasts.
Signs & Symptoms of Rheumatoid Arthritis
The most common and prominent symptoms are joint pain and swelling, which usually appear gradually over several weeks to months.
The small joints of the hands and feet are typically the first to be affected, followed by larger joints.
The presence of synovitis, manifested as soft tissue swelling or effusion of the affected joint, is a key feature of RA in early disease.
Morning stiffness in the affected joints, as well as local soft tissue swelling, warmth, and redness.
Three or more joints are typically impacted at once.
Patients commonly report fatigue, anorexia, and weight loss.
Fever can occur as a direct result of the disease, but temperatures above 38.0°C usually indicate concurrent infection.
Causes of Rheumatoid Arthritis
In many cases, it is caused by the interaction of genes and environmental factors, including tobacco.
RA is caused by an immune response in which the body’s immune system attacks its healthy cells.
Although the exact causes of RA are unknown, certain factors can raise the risk of the condition.
Risk Factors of Rheumatoid Arthritis
Gender → Rheumatoid arthritis occurs 2–3 times more frequently in women than in men. The period immediately following pregnancy is the highest risk for developing initial symptoms.
Age → In both sexes, the incidence rises with age up to the seventh decade. Peak onset occurs between the ages of 35 and 64 for both sexes.
Genetics → People who are born with certain genes are more likely to develop RA. These genes, known as HLA (human leukocyte antigen) class II genotypes, can also worsen your arthritis.
There is a higher incidence in identical twins than in non-identical twins, and there is a higher incidence and severity in first-degree relatives of rheumatoid arthritis patients.
Environmental influences → Bacterial and viral infections that have been linked with triggering rheumatoid arthritis include parvovirus, rubella virus, Mycoplasma, Epstein-Barr virus (EBV), and cytomegalovirus.
Obesity → Studies examining the impact of obesity also discovered that a person’s risk of developing RA increased with increasing weight.
Other influences → Lower socioeconomic status, lower education levels, and lower levels of psychosocial well-being. Smoking is linked to both a higher incidence and a more severe disease.
Diagnosis of Rheumatoid Arthritis
RA is diagnosed through a review of symptoms, a physical examination, and X-rays and lab tests.
It is best to identify RA early—within six months of the onset of symptoms—so that patients can start treatment to slow or stop the disease’s progression (for example, damage to joints).
a. Typical Presentation
RA patients often experience pain and stiffness in several joints.
The most commonly affected joints are the wrists, proximal interphalangeal joints, and metacarpophalangeal joints.
Morning stiffness that lasts more than an hour suggests an inflammatory cause.
On joint examination, boggy swelling due to synovitis may be visible, or subtle synovial thickening may be palpable.
Patients may also experience more indolent arthralgias before clinically visible joint swelling.
With active disease, systemic symptoms such as fatigue, weight loss, and low-grade fever may occur.
b. Diagnostic Criteria
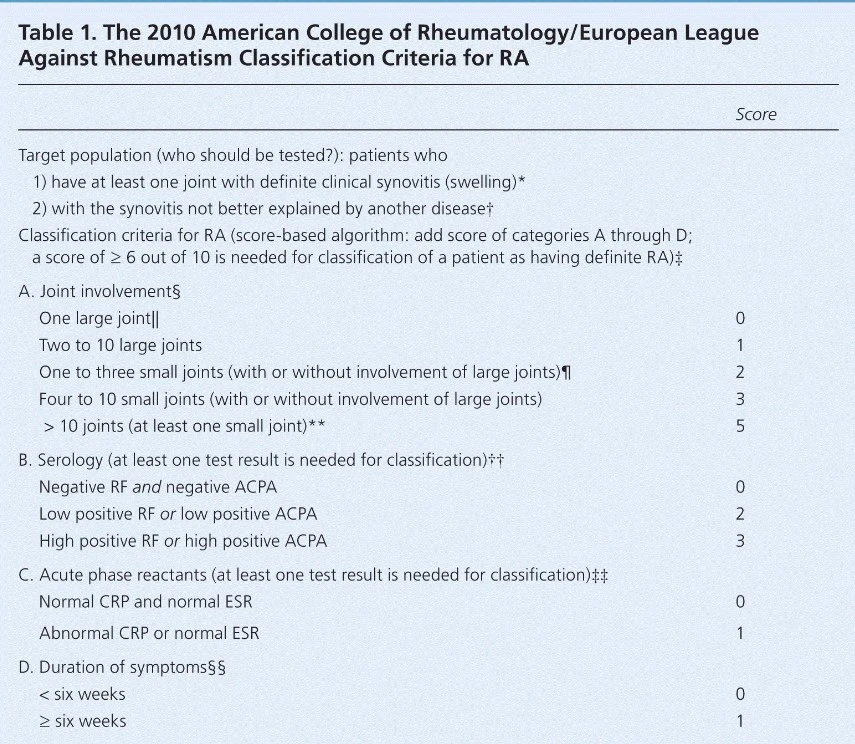
The 2010 American College of Rheumatology/European League Against Rheumatism Classification Criteria for RA
c. Diagnostic Tests
Autoantibodies are commonly found in autoimmune diseases such as RA.
Rheumatoid factor, anti-citrullinated protein antibody, or both are present in 50–80% of people with RA.
Antinuclear antibody testing can be positive in RA patients, and it’s important for prognosis in juvenile forms of this disease.
C-reactive protein levels and erythrocyte sedimentation rate are commonly elevated in active RA, and these acute phase reactants are part of the new RA classification criteria.
C-reactive protein levels and erythrocyte sedimentation rate can also be used for monitoring disease activity and medication response.
The results of a baseline complete blood count with differential and an assessment of renal and hepatic function are useful because they may affect treatment choices.
Complications of Rheumatoid Arthritis
- Premature death.
- Serious infections.
- Osteopenia and osteoporosis are disease-related complications that can also be linked to drug therapies (glucocorticoids).
- RA patients are more likely to develop venous thromboembolic disease.
- Depression is a major complication of RA. It is found in patients who have long-term active disease and severe physical dysfunction.
- Premature heart disease. People who have RA are also more likely to develop other chronic diseases like heart disease and diabetes.
- Employment. RA can make it difficult to work. Adults with RA are less likely to be employed than non-RA adults.
Life Expectancy of Rheumatoid Arthritis
RA can shorten your life expectancy.
The average life span of RA patients was 65.8 years in males and 63.7 years in females, which is much shorter than the general population.
Cardiovascular disease was the leading cause of death.
Read Also: SAPHO Syndrome | Causes, Symptoms, Diagnosis & Treatments
Treatment & Management of Rheumatoid Arthritis
Rheumatoid arthritis management can be divided into three categories: –
- Using analgesics to manage pain.
- Disease management using DMARDs or biological DMARDs (including bridging therapy and corticosteroid for flare control).
- Aggressive control of co-morbidities, such as cardiovascular risk factors.
Medicines used to manage the disease process in rheumatoid arthritis are classed into three distinct categories: –
- Analgesics.
- Corticosteroids.
- DMARDs, including biological DMARDs.
1. Analgesics
Analgesics are used to treat pain and inflammation, which are major concerns for RA patients.
Although paracetamol continues to be the preferred analgesic due to its excellent safety profile, NSAIDs like ibuprofen, diclofenac, or celecoxib are most frequently used to treat these symptoms in the beginning.
Traditional and COX-2 selective NSAIDs are more effective than simple analgesics in alleviating the signs and symptoms of active disease, but this must be balanced against the potential gastrointestinal, renal, and cardiovascular side effects of this class of drugs.
In late disease, inflammation is less noticeable and pain is linked to structural joint damage, so paracetamol may be used instead of NSAIDs at this point.
To manage more severe pain, opioid analgesics are sometimes required.
Fatty acid supplements (omega-3 and gamma-linolenic acid) may help reduce pain and inflammation in RA patients.
Fish oils have been shown to lower blood pressure, improve arterial compliance, and reduce elevated triglycerides. They may also reduce the production of pro-inflammatory eicosanoids and cytokines.
There is high-quality evidence to support the benefits of high-dose omega-3 polyunsaturated fatty acids (up to 12 fish oil capsules or 15 mL liquid fish oil) in RA for reducing pain, morning stiffness, the number of painful or tender joints, and NSAID use.
2. Corticosteroids
Corticosteroids control severe joint inflammation in early disease or active flares rapidly and effectively.
They are important drugs because they have anti-inflammatory and immunosuppressive properties, as well as disease-modifying activity, which helps to control joint inflammation, improve physical function, and slow the progression of joint damage.
Corticosteroid bridging therapy uses short-term glucocorticoid administration to provide rapid disease control until the less toxic DMARDs can take effect.
Oral corticosteroids such as prednisone and prednisolone are used to treat rheumatoid arthritis in three ways: –
- As a starting bridging therapy until DMARDs start working.
- managing sudden flare-ups.
- When DMARD therapy is inadequate, it is used in conjunction with DMARDs, and it is sometimes used as the sole therapy.
3. Disease-modifying anti-rheumatic drugs (DMARDs)
DMARDs are the mainstay treatment for RA because of their ability to modify the disease and favorable toxicity profile.
Only DMARDs and b-DMARDs are capable of preserving joint function, easing symptoms, and inducing clinical remission while still maintaining a respectable long-term safety profile.
As soon as a diagnosis is made, DMARDs should be started; they are no longer delayed until radiographic deterioration.
Methotrexate is the first-line treatment for RA.
Depending on the disease’s severity, sulfasalazine, hydroxychloroquine, or leflunomide may be used in place of or in addition to methotrexate.
Biological DMARDs are a relatively new therapy in RA and have been used successfully in combination with traditional DMARDs.
DMARDs and b-DMARDs available for the treatment of rheumatoid arthritis
a. DMARDs
- Azathioprine.
- Cyclosporin.
- Cyclophosphamide.
- Hydroxychloroquine.
- Leflunomide.
- Gold salts.
- Methotrexate.
- Sulfasalazine.
b. Biological DMARDs
- TNF-α inhibitors.
- Adalimumab.
- Infliximab.
- Etanercept.
Cytokine Modulators.
- Rituximab.
- Anakinra.
- Abatercept.
4. Physical Therapy
Randomized controlled trials show that physical exercise can improve the quality of life and muscle strength in RA patients.
Although randomized trials are limited, Tai Chi has been shown to improve ankle range of motion in people with RA.
5. Joint Replacement
When medical management fails to control symptoms and there is severe joint damage, joint replacement is recommended.
The hip and knee are the most common joints to be replaced.
Related Content: Early Signs of Lupus in Females
Summary
Rheumatoid arthritis is a progressive, chronic, and degenerative autoimmune inflammatory disease that is primarily characterized by synovitis.
It is a chronic systemic inflammatory disorder marked by inflammation of the surrounding tissues, including tendons, ligaments, and muscles, as well as deformity of the synovial joints.
RA is caused by an immune response in which the body’s immune system attacks its healthy cells.
In RA, the immune and inflammatory systems play a crucial role in the destruction of bone and cartilage.
Rheumatoid factor (RF) and anti-citrullinated protein antibodies (ACPAs) are produced in RA and are targeted against autoantigens that are commonly found within and outside of synovial joints.
Signs and symptoms of RA include: –
- Pain or aching in more than one joint.
- Stiffness in more than one joint.
- Tenderness and swelling in more than one joint.
- The same symptoms on both sides of the body (such as in both hands or both knees).
- Weight loss.
- Fever.
- Fatigue or tiredness.
- Weakness.
The small joints of the hands and feet are typically the first to be affected, followed by larger joints.
RA is diagnosed through a review of symptoms, a physical examination, and X-rays and lab tests.
It is best to identify RA early—within six months of the onset of symptoms—so that patients can start treatment to slow or stop the disease’s progression (for example, damage to joints).
Medicines used to manage the disease process in rheumatoid arthritis are classed into three distinct categories: –
- Analgesics.
- Corticosteroids.
- DMARDs, including biological DMARDs.
References
- G.M., L., & C., S. (1970, January 1). Rheumatoid arthritis. SpringerLink. from Springer Link
- Radu, A.-F., & Bungau, S. G. (2021, October 23). Management of rheumatoid arthritis: An overview. Cells. from PubMed
- (PDF) rheumatoid arthritis – researchgate. from ResearchGate
- Rheumatoid arthritis – statpearls – NCBI bookshelf. from PubMed
- Centers for Disease Control and Prevention. (2020, July 27). Rheumatoid arthritis (RA). Centers for Disease Control and Prevention. from CDC
- [PDF] managing patients with rheumatoid arthritis – researchgate. from ResearchGate
- (PDF) therapeutic strategies for rheumatoid arthritis – researchgate. from ResearchGate
- Wasserman, A. M. (2011, December 1). Diagnosis and management of rheumatoid arthritis. American Family Physician. from American Academy of Family Physicians
- (PDF) rheumatoid arthritis – researchgate. from ResearchGate
- Yoshizawa H;Kudo H;Iwano K;Yamada A;Aikawa T;Miyamoto Y;Takahashi K;Saito K;Ogita T;Okudaira K; (n.d.). [causes of death in patients with rheumatoid arthritis–analysis of 117 cases for 13 years]. Ryumachi. [Rheumatism]. from PubMed
- Minaur NJ;Jacoby RK;Cosh JA;Taylor G;Rasker JJ; (n.d.). Outcome after 40 years with rheumatoid arthritis: A prospective study of function, disease activity, and mortality. The Journal of rheumatology. Supplement. from PubMed