People who abuse alcohol are typically at risk for a wide range of alcohol-related medical complications. Alcohol has a variety of negative effects on blood...
Pernicious Anemia | Causes, Symptoms, Diagnosis & Treatments
What is Pernicious Anemia?
Pernicious anemia (PA) is an autoimmune condition with a multifactorial etiology that includes environmental and immunological factors.
It is the leading cause of cobalamin deficiency anemia globally.
The disease is macrocytic anemia caused by a vitamin B12 deficiency, which is caused by an intrinsic factor (IF) deficiency.
Pernicious anemia is a relatively rare condition, with a prevalence of less than 1% in European-ancestry populations.
Pernicious anemia is a common cause of megaloblastic anemia worldwide; it affects people of all ages, but especially those aged 60-70 (2% prevalence).
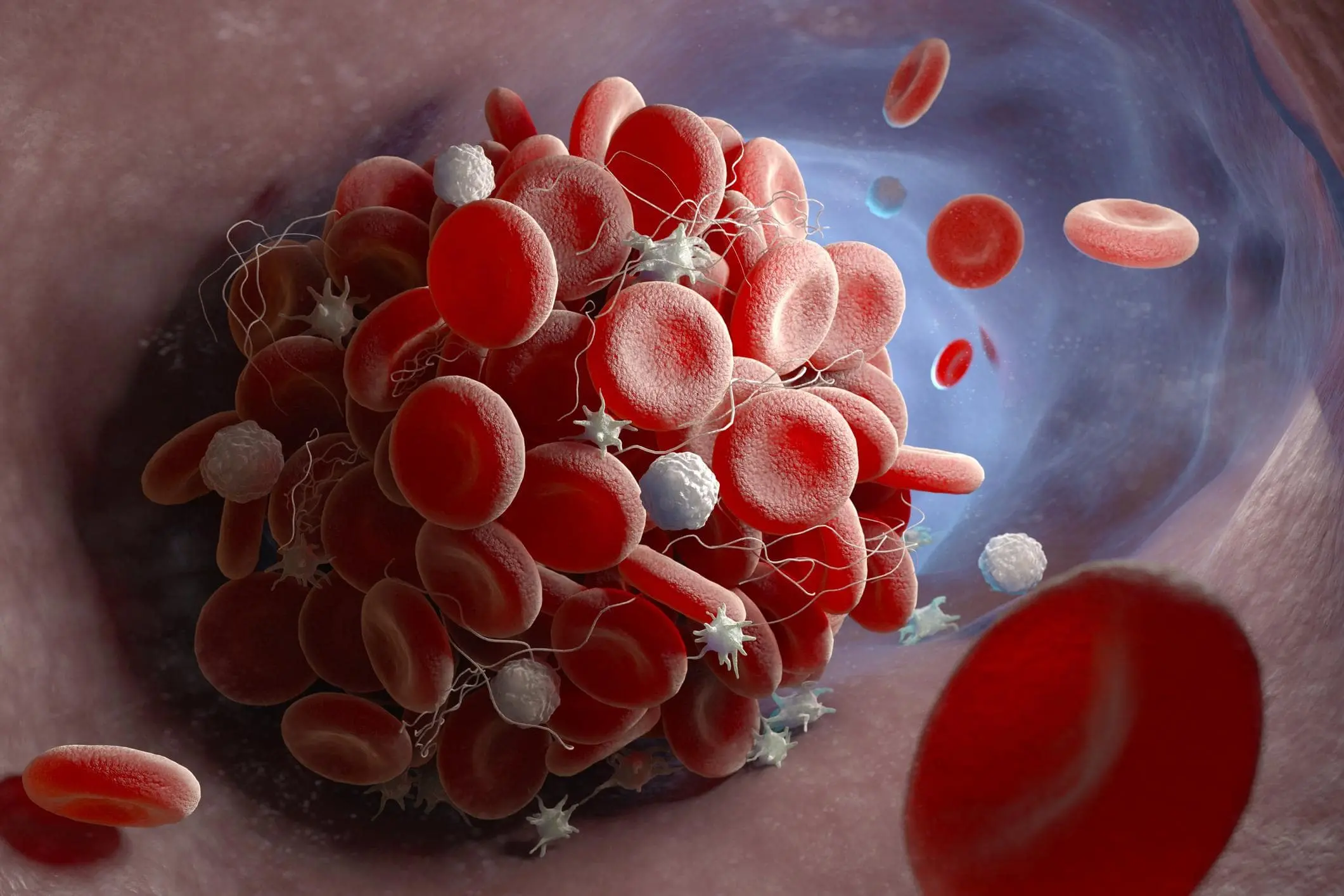
Pathophysiology of Pernicious Anemia
The primary pathophysiological mechanism in pernicious anemia is decreased dietary B12 absorption due to IF deficiency.
All formed blood components experience megaloblastic changes as a result of B12 deficiency, but erythrocytes exhibit the most serious changes, with the severity of red blood cell morphologic changes corresponding to the severity of anemia.
Causes of Pernicious Anemia
Pernicious anemia is a complicated condition with an obvious autoimmune origin.
The anemia is megaloblastic and is caused by a deficiency of vitamin B12, which is secondary to intrinsic factor (IF) deficiency.
A glycoprotein called IF, which is produced and secreted by parietal cells, binds to vitamin B12 and helps to transport it to the terminal ileum for absorption.
Anti-IF antibodies prevent the binding of B12 to IF, which prevents the formation of the B12/IF complex, or binding to the B12/IF complex, which prevents intestinal absorption.
Pernicious anemia can be found in up to 25% of people who have autoimmune gastritis (AIG), which affects the corpus and fundus and spares the antrum.
Anti-parietal cell antibodies destroy parietal cells found only in the oxyntic mucosa, which produce IF and hydrochloric acid.
As a result of achlorhydria, the release of cobalamin bound to dietary protein decreases, and fewer parietal cells are available to produce the IF required for dietary B12 absorption.
Five genome-wide significant signals for pernicious anemia have been found, indicating genetic risk factors.
It is unknown whether Helicobacter pylori is a contributing factor to pernicious anemia.
Symptoms of Pernicious Anemia
clinical B12 deficiency.
As compensatory cardiopulmonary mechanisms enable increases in oxygen delivery, symptoms may not appear until the anemia is relatively severe.
The clinical presentation is gradual, and patients typically exhibit symptoms of:-
- Anemia with pallor.
- Fatigue.
- Lightheadedness.
- Tachycardia and decreased mental concentration.
Small-bowel epithelial involvement can cause malabsorption and diarrhea, as well as weight loss and anorexia.
Glossitis is a common sign of megaloblastic anemia, and the patient has a painful, smooth, red tongue.
Other symptoms include early satiety, epigastric discomfort, postprandial bloating, and dyspeptic symptoms.
Neurological Symptoms of Pernicious Anemia
Vitamin B12 deficiency causes neurologic abnormalities in PA.
Neurological symptoms include the following: –
- Paresthesia.
- Unsteady gait.
- Clumsiness.
- Dementia.
- Ataxia.
- Optic atrophy.
- Psychosis.
- Mood disturbance.
- Spasticity in some cases.
Indeed, vitamin B12 deficiency can cause peripheral neuropathy as well as lesions in the posterior and lateral columns of the spinal cord (subacute combined degeneration) and the cerebrum.
These lesions progress from demyelination to axonal degeneration and eventually neuronal death.
It is crucial to identify these signs as soon as possible because, even with vitamin B12 replacement therapy, the neurological lesions might not be reversed.
Diagnosis of Pernicious Anemia
PA is defined as a hemoglobin concentration of 13 g/dL for men and 12 g/dL for women, a mean corpuscular volume of ≥ 100 fL, low levels of cobalamin (vitamin B12), and the presence of ABG and intrinsic factor deficiency.
PA is diagnosed by the presence of megaloblastic anemia, low serum vitamin B12 levels, gastric atrophy, and the presence of antibodies to the gastric parietal cell, or IF.
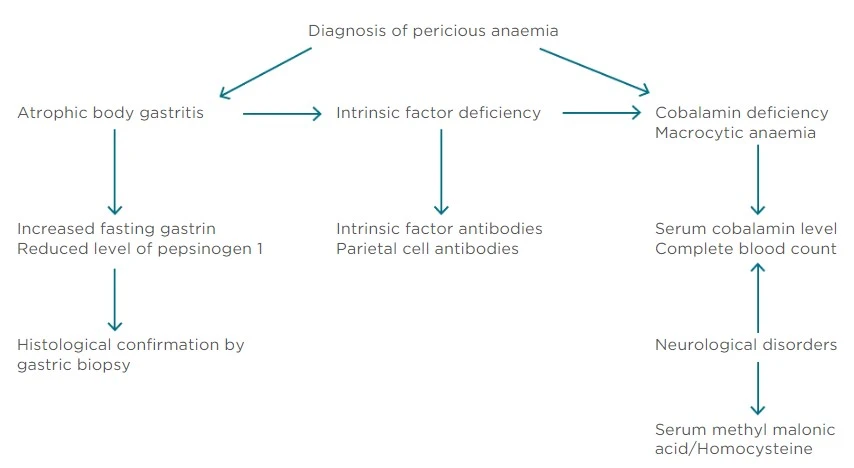
Diagnostic algorithm for pernicious anemia
Life Expectancy of Pernicious Anemia
Early detection and treatment of pernicious anemia now results in a normal, and usually uncomplicated, lifespan.
Delayed treatment allows the anemia and neurologic complications to worsen.
Neurologic complications may become permanent if patients are not treated at an early stage of the disease.
Treatments for Pernicious Anemia
The clinical management of PA patients is divided into two parts: treatment of cobalamin deficiency and monitoring of iron deficiency onset.
There are different therapeutic recommendations for PA in terms of the dosage and administration of vitamin B12 replacement therapy.
Vitamin B12 must be administered parenterally, and patients typically receive an intramuscular injection of 1,000 g B12 every day or every other day during the first week of treatment.
The following month, they will receive injections every week, followed by monthly injections.
Although PA requires lifelong treatment and supplementation increases the percentage of vitamin B12 absorption, symptoms of vitamin B12 deficiency may improve with just a few days of medical treatment. However, cobalamin does not cure gastric atrophy.
Summary
Pernicious anemia (PA) is an autoimmune condition with a multifactorial etiology that includes environmental and immunological factors.
It is the leading cause of cobalamin deficiency anemia globally.
The primary pathophysiological mechanism in pernicious anemia is decreased dietary B12 absorption due to IF deficiency.
Pernicious anemia is a complicated condition with an obvious autoimmune origin.
The anemia is megaloblastic and is caused by a deficiency of vitamin B12, which is secondary to intrinsic factor (IF) deficiency.
The clinical presentation is gradual, and patients typically exhibit symptoms of:-
- Anemia with pallor.
- Fatigue.
- Lightheadedness.
- Tachycardia and decreased mental concentration.
PA is diagnosed by the presence of megaloblastic anemia, low serum vitamin B12 levels, gastric atrophy, and the presence of antibodies to the gastric parietal cell, or IF.
Early detection and treatment of pernicious anemia now results in a normal, and usually uncomplicated, lifespan.
Delayed treatment allows the anemia and neurologic complications to worsen.
The clinical management of PA patients is divided into two parts: treatment of cobalamin deficiency and monitoring of iron deficiency onset.
There are different therapeutic recommendations for PA in terms of the dosage and administration of vitamin B12 replacement therapy.
Vitamin B12 must be administered parenterally, and patients typically receive an intramuscular injection of 1,000 g B12 every day or every other day during the first week of treatment.
How useful was this post?
Click on a star to rate it!
Average rating 0 / 5. Vote count: 0
No votes so far! Be the first to rate this post.
I'm sorry that this post was not useful for you!
Let me improve this post!
Tell me how I can improve this post?
References
- National Center for Biotechnology Information. PubMed
- Pernicious anaemia: Mechanisms, diagnosis, and management – researchgate. ResearchGate
- Pernicious anemia: New insights from a gastroenterological point of view. ResearchGate
- Srikanth Nagalla, M. (2022, June 29). Pernicious anemia. Practice Essentials, Pathophysiology, Etiology. Medscape
Macrocytic anemia is defined as macrocytosis (mean corpuscular volume (MCV) greater than 100 fL). Macrocytosis affects 2% to 4% of the population, 60% of whom...
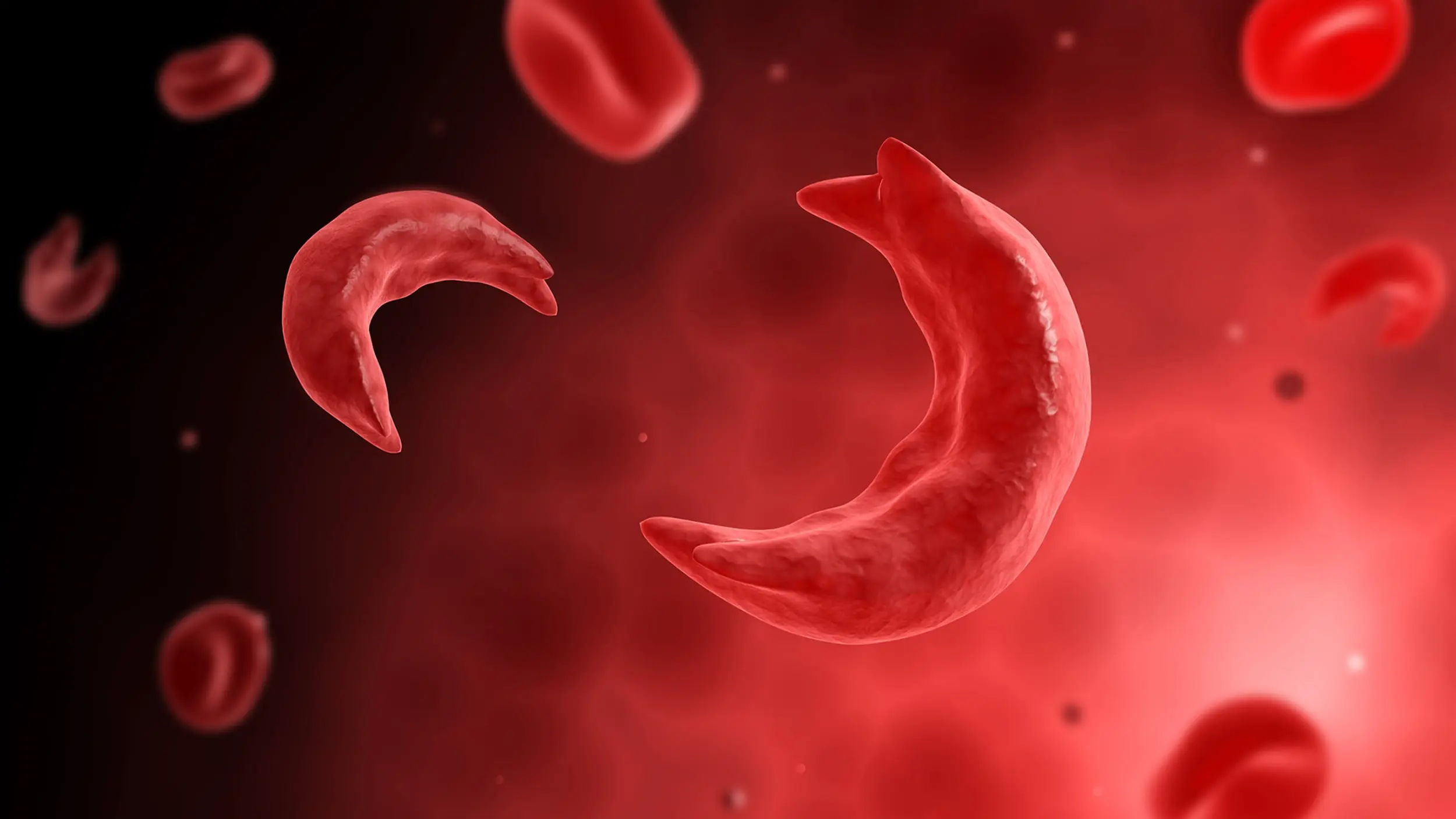
Sickle Cell Anemia | Causes, Symptoms, Diagnosis and Treatments
Sickle cell anemia is an inherited condition of the globin chains that leads to hemolysis and chronic organ damage.
Microcytic anemia is caused by insufficient hemoglobin (Hb) formation in erythroid precursors, resulting in a decrease in red blood cell mean corpuscular volume (MCV). These...
Featured Posts
Recent Posts
Popular Posts
Learn More